Chief Quality Officer at Ascension and Executive Vice President and Chief Clinical Officer at Ascension
 Illustration by Andrew Baker
Illustration by Andrew BakerWhen people first arrive at one of our hospitals, many may be experiencing some of the worst, most vulnerable times of their lives — or the life of a loved one. They may feel anxious and afraid of what might happen next. They put their lives in
our hands, trusting in the safe, quality care they will receive. They also often come with a set of unspoken expectations: please keep me safe; help me navigate my care; provide me with the right care; give me tools to help me stay well; and treat
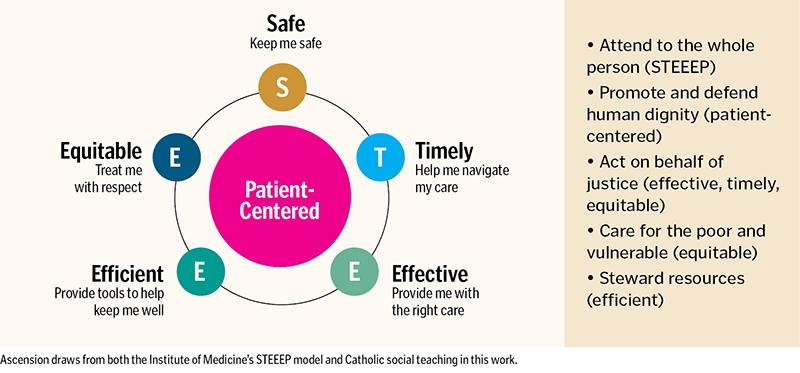
me with respect. For years, the "safe, timely, effective, efficient, equitable and patient-centered" (STEEEP) model, developed by the Institute of Medicine,1 has provided a clear and actionable framework to help Ascension manage overall
quality and safety initiatives. Each element of the STEEEP framework has multiple metrics that we report and track over time.
Upon deeper reflection on this framework, we began to see its inherent ties to Catholic social teaching. Through STEEEP, we attend to the whole person and put the patient at the center of all we do as a way to promote and defend human dignity. When we
ensure our care is effective, timely and equitable, we act on behalf of justice. As we find ways to make care more efficient, we become better stewards of our resources. And when we provide equitable care, we fulfill our mission to provide care to
all, especially for those who are poor and vulnerable. In these ways and more, Catholic health care's identity inspires and drives our resolute commitment to quality care.
This framework was challenged for Ascension and other health systems across the country during the COVID-19 pandemic — impacting processes, workflows, supply chain, the workforce and more. Hospitals encountered record numbers of seriously ill patients,
requiring complex care and support. Health systems needed a new playbook. And with our enduring mission to sustain and improve the health of individuals and communities in mind, we set out to optimize the care we provided, including our ongoing commitment
to quality and safety.
RECOGNIZE AND RESCUE
In January 2022, Ascension implemented at all its hospitals an initiative called Recognize and Rescue, which has helped save nearly 3,000 additional lives. The unique approach to optimize quality and safety across
our ministry involves recognizing problems before they happen, then rescuing patients if problems arise. The initiative is organized into two components:
• The Recognize component consists of identifying high-risk conditions, situations and medications and preventing adverse events. Focus areas include: implementing risk-reduction strategies for health care-associated infections, mitigating medication
risks, improving the management of sepsis, optimizing the management of patients with respiratory compromise and practicing person-centered engagement.
• The Rescue component consists of identifying early when a patient begins to decline and promptly intervening to support improvement in health and function. Focus areas include: standardizing rapid response team and code team protocols and processes,
encouraging escalation and use of chain of command for concern resolution, prioritizing frontline health care worker education and promoting teamwork.
COLLABORATION KEY TO SUSTAINABLE IMPROVEMENT
Ascension's Recognize and Rescue initiative provides a foundation for anchoring standardized processes in care, reducing variation and promoting optimal outcomes in the acute care setting
across 12 markets. We achieved this goal through a coordinated, systemwide adoption of a collaborative approach. Promoting teamwork through multidisciplinary partnership was the linchpin that made the adoption of these quality and safety improvement
efforts possible. We built a structure to support the work by establishing both system and market teams. Teams in our sites of care brought together multiple disciplines, including physicians, nurses and those working in infection prevention, respiratory
therapy, pharmacy, analytics, education, consumer experience, environmental services, risk, and quality and patient safety. We tailored our interventions to hospitals with the greatest opportunities and ensured Recognize and Rescue was integrated
into market and hospital-level quality efforts and did not duplicate other initiatives.
Successful adoption of the program was made possible with tools used in carrying out a gap analysis, actionable data to help identify focus areas and clear accountability for performance. Process and outcome measures were set to help identify opportunities
at the market and hospital levels as well as intra-institutional opportunities at the provider level. System, market and hospital-level accountability was clearly defined, involving physicians, nurses and pharmacists. Partnering with our analytics
team, we established and published a monthly updated dashboard for process and outcome measures, with feedback on performance at the hospital, market and system levels.
OUR OUTCOMES
The Recognize and Rescue initiative has enhanced quality and safety across all of our hospitals. We view this approach as a conduit to optimize outcomes and sustain future gains. Through a bundle of aligned interventions,
all 12 of our markets with 94 participating hospitals showed sustainable improvements in lives saved and safety events. The graphic on page 27 illustrates how our mission to improve quality and safety has been impacted by Recognize and Rescue thus
far.
Effective Care
With the goal of optimizing patient outcomes, we focused on conditions associated with higher mortality, such as sepsis or patients presenting with respiratory symptoms. Integrating a standardized approach for identifying
and managing sepsis and encouraging the use of standardized order sets supported a reduction in care variations and led to better outcomes. In addition, we worked on refining the process to ensure appropriate medical, nursing and level of care support
was provided to patients presenting with respiratory symptoms. Altogether, such interventions not only helped to improve our outcomes, but also helped us save more lives and anchor our standardized processes in care.
Equitable Care
Exploring results through a health equity lens, we see that our patients who identify as white and our patients who identify as Black have comparable outcomes, which underscores our goal of reducing disparities in
care. This was similar during the pandemic, when we witnessed no difference in mortality in COVID-19-infected patients who identified as either white or Black after we adjusted for differences in sociodemographic and clinical factors.2 Identifying social determinants of health is one meaningful way to reduce preventable disparities in health outcomes. Ascension Medical Group has implemented a standardized screening tool, exceeding more than 2 million screenings.
Safe Care
The remaining four bars shown on the graph below represent common industry-wide, frontline quality measures that, when managed well, can help keep patients safe from these infections:
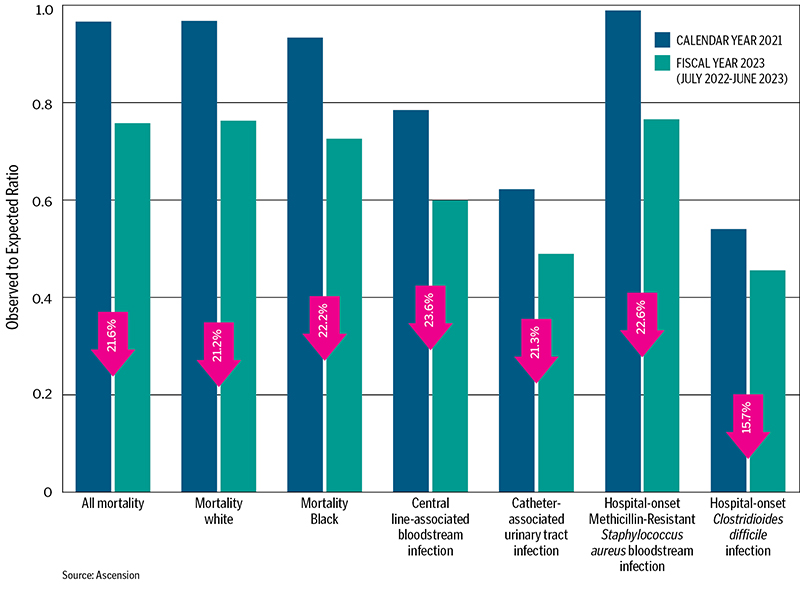
CLABSI: Central line-associated bloodstream infection
CAUTI: Catheter-associated urinary tract infection
HO MRSA: Hospital-onset Methicillin-Resistant Staphylococcus aureus bloodstream infection
HO C. Difficile: Hospital-onset Clostridioides difficile infection
We instituted multiple measures to reduce health care-associated infections, with close attention to improving competencies of frontline workers by managing patients with central lines and urinary catheters, using checklists to conduct gap analyses and
providing regular feedback to teams on their performance. The teams developed action plans for any gaps identified, and senior leaders were accountable for the outcomes.
IMPLEMENTING RECOGNIZE AND RESCUE
The Recognize and Rescue approach was designed to be replicable. Prior to adoption and implementation, health systems should ask the following questions:
- How should we structure our team at the system, market and hospital level, and who are our key stakeholders? For successful implementation, organizations will need to convene a team of experts — including physicians, nurses
and other health care professionals — with the support of a leader to push for accountability. The Recognize and Rescue toolkit provides the technical information to guide teams on how to implement best practices. Many members are content
experts who help provide direction to the market teams on improvement recommendations. Market-based teams are responsible for the work, and a team representing each hospital may be required to ensure goals are achieved, led through a partnership
between the chief medical and nursing officers.
- How can we effectively implement standardized processes and efficiently provide feedback on performance? For productive implementation, it is essential to ensure that support for education and evaluation of performance is in place,
especially for measures that are sensitive to frontline caregiver performance, such as for central line-associated bloodstream infections.
- How will we extract data, measure success and communicate outcomes? Most of the outcome data are publicly reported and easily accessible to any system. However, some other processes or intermediate outcomes may require data feeds
from electronic health records. Establishing a dashboard for process and outcome measures that allows trending is also important. We were able to share provider-level data for some measures, which enhanced local engagement.
- How should we establish expectations and clear lines of accountability? For each element of the initiative, owners are clearly identified from system, market and hospital levels and are accountable for their performance. The system
team engages the hospitals by providing details on measures of opportunities and may also help offer technical solutions.
- How can we ensure our approach is sustainable? In parallel with the implementation of the Recognize and Rescue initiative, our teams continue to enhance the work of standard quality and safety evaluations through reviews and root
cause analyses for safety events.
QUALITY MEASURES, EFFECTIVE CARE
Recognize and Rescue provides an innovative approach to adopt and cascade quality improvement efforts by having clear elements to implement, coupled with the use of robust data for both processes
and outcomes. Through this initiative's focus on building structures, standardizing processes, providing feedback on performance and ensuring accountability, sustainable improvements transpired around reductions in mortality and infections and the
practice of better safety measures. By honoring our commitment to deliver quality treatment, we can help to ensure that all our patients receive equitable and dignified care to continue living longer and healthier lives.
MOHAMAD FAKIH serves as chief quality officer at Ascension. RICHARD FOGEL serves as executive vice president and chief clinical officer at Ascension.
NOTES
- "Six Domains of Healthcare Quality," Agency for Healthcare Research and Quality, https://www.ahrq.gov/talkingquality/measures/six-domains.html.
- Baligh R. Yehia et al., "Association of Race with Mortality among Patients Hospitalized with Coronavirus Disease 2019 (COVID-19) at 92 U.S. Hospitals," JAMA Network Open 3, no. 8 (August 18, 2020): https://doi.org/10.1001/jamanetworkopen.2020.18039.